Information for Health Care
Providers
Distinguishing Between
Influenza-like Illness
and Early Inhalation Anthrax
In most circumstances, the
Illinois Department of Public Health does not make specific recommendations
about patient care. However, it is providing the following information, which
may help with clinical decisions. Ultimately, though, clinical decisions about
patient care remain with the health care provider.
It is important that health
care providers follow reporting requirements. When a diagnosis of a
bioterrorism-associated illness is suspected, it is critical that the case be
reported to the local health department within three hours of such
recognition.
1. Health care providers
should review the Morbidity and Mortality Weekly Report (November 2,
2001).
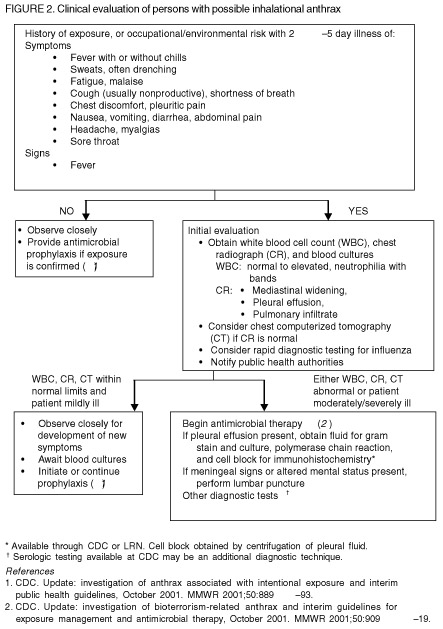
Of particular importance is
the flow diagram on page 945 (Figure 2, reproduced below). Additional guidance
from the U.S. Centers for Disease Control and Prevention (CDC) can be found in
the November 9, 200, issue (Vol. 50, No. 44) of the MMWR. Another article of
interest will appear in the November 29, 2001, issue of the New England
Journal of Medicine: “Recognition and management of anthrax - an
update” by M.N. Swartz.
2. Anthrax is rare and
influenza-like illnesses are common.
Although the symptoms of
influenza and influenza-like illnesses may overlap with the early presentation
of inhalation anthrax, it should be emphasized that influenza is primarily an
upper respiratory tract infection (e.g., cough and sore throat) with
accompanying fever, headache, myalgia and malaise but with a wide spectrum of
severity. Recently reported cases of inhalation anthrax , a lower respiratory
tract infection, may have minimal or nonproductive cough but frequently have
chest discomfort or pleuritic pain. When influenza is complicated by lower
respiratory tract findings, such as pneumonia, then differentiating from
anthrax may be more difficult. Whenever inhalation (or any form of) anthrax is
being considered, consultation with an infectious disease physician is
recommended.
Based on review of the
relatively few published cases of inhalation anthrax and the recent
bioterrorism-related cases, rhinitis is rarely, if ever, seen with anthrax. Its
presence, therefore, is a possible clue that influenza or influenza-like
illness is present; however, its absence is of no value because many cases of
influenza and influenza-like illnesses will not have rhinitis.
Symptoms such as fever,
sweats, chills, myalgias, fatigue, malaise, dry cough, headache and sore throat
may occur in either illness, so their presence or absence is of no value. But
the rarity of anthrax and the relative frequency of influenza and
influenza-like illnesses should be considered when doing a diagnostic
evaluation, just as the incidence of illnesses guides other decisions in
clinical medicine. Clinicians should avoid letting fear obscure sound clinical
judgment.
There are no early laboratory
clues that can be considered diagnostic. It has been noted that none of the
inhalation anthrax cases had a low white blood cell count. This information
cannot be reliably used to differentiate anthrax from other illnesses since it
is possible that anthrax could infect someone who already has a low white blood
cell count (e.g., an immunocompromised person). Also, the number of studied
anthrax cases is still relatively small, so generalizations about the disease
are limited.
3. Occupation and exposure
history should be obtained to help assess the relative risk of anthrax in an
individual presenting with influenza-like illness.
To date, nearly all cases of
inhalation anthrax have been either a postal worker, a mail handler or sorter,
or a recipient of an envelope containing anthrax spores. For a few additional
cases, the exposure has not been determined but those investigations are
ongoing. Therefore, risk is certainly increased if someone is linked to one of
the confirmed anthrax events in the District of Columbia, Florida, New Jersey
or New York City. And, heightened concern is reasonable if dealing with persons
who handle mail or who have been exposed through an incident that appears to be
credible or that was determined by law enforcement to be credible and for which
laboratory evidence has not ruled out anthrax.
4. Rapid influenza tests may
be performed to help evaluate a case of anthrax versus influenza.
Such testing has limitations
that do not make it reliable for this purpose. While makers of the rapid
influenza tests report overall sensitivity of 70 percent and specificity of 90
percent, these are likely overestimates based on unpublished data of which the
CDC is aware. In fact, it is not unusual for rapid influenza tests to yield
false positives and false negatives. During peak flu season, only one-third of
influenza-like illnesses submitted for viral testing actually test positive for
influenza. The positive predictive value of these tests suffer during non-peak
portions of the flu season. So, a negative rapid influenza test does not mean a
person has anthrax.
5. To date, there have been no
cases of anthrax nor environmental test results positive for anthrax in
Illinois.
Millions of cases of
influenza-like illness occur every year. Therefore, while public health
officials and health care providers need to be in a state of heightened
awareness for anthrax, it is important to keep in mind that, for any individual
case, the odds are very small that it is truly anthrax.
6. If diagnostics are
performed to evaluate a possible human case of anthrax, such specimens should
be initially processed in a local hospital or other qualified laboratory,
unless such testing requires specialty techniques such as PCR or
immunohistochemical testing of tissue.
If test results suggest the
presence of a Bacillus species that may be B. anthracis, then the
local health department should be notified immediately so that staff can
consult with IDPH laboratory personnel or the Department’s infectious
disease staff about forwarding such specimens to the state laboratory for
confirmation or speciation.
|